

Document Type : Original Article
Authors
1 Zoology Department, Gombe State University, Gombe, Nigeria
2 Preliminary and general Studies department, Federal College of Horticulture Dadin Kowa, Gombe State, Nigeria
3 Department of Microbiology, Federal University Dustin-Ma, Kastina State, Nigeria
Abstract
Keywords
Sub-Saharan Africa suffers most from the catastrophic effects of malaria, with approximately 93% of the global malaria cases and nearly 94% of deaths, making the disease a severe economic and public health burden [1]. Plasmodium falciparum, Plasmodium vivax, Plasmodium malariae, and Plasmodium ovale are the four species responsible for the infection. These four species are transmitted through the bite of an infected female Anopheles mosquito [2], and the majority (99%) of malaria in Sub-Saharan Africa is caused by Plasmodium falciparum [3].
Over 125 million pregnant women are annually exposed to malaria worldwide, and roughly 25% of infections occurring in Africa are among pregnant women [4][5]. Pregnant women and children under the age of five are especially susceptible to malaria in Nigeria and other malaria-endemic countries, partly because of lowered immunity [6][7]. Severe anemia [8], maternal fatalities, low birth weight, and stillbirth are some of the adverse effects of malaria in pregnancy [9]. Most importantly, malaria infection is responsible for 70% of all deaths in these populations [10].
The susceptibility and severity of malaria infection in pregnant women are influenced by a number of biological factors, including immunological and humoral changes, parity, maternal age, gestational age, and transmission intensity [11]. Additionally, erythrocyte polymorphisms, including the ABO blood classes, are related to the clinical outcome of falciparum malaria in endemic locations. Human erythrocytes and other cells have several carbohydrate antigens that make up the ABO blood group [12]. In many regions where the disease is endemic, the impact of ABO blood types on malaria in pregnancy continues to be enigmatic. Studies of malaria parasitemia from that standpoint in populations of malaria endemic regions will help elucidate any such relationship. It is believed that knowing the relationship nature (if any) between ABO blood groups and malaria parasitemia would provide an invaluable window into the scourge. Due to the dearth of data from the chosen study area (Kwadon, Yamaltu-Deba), the investigation was necessary. Therefore, this study aimed to ascertain the prevalence of malaria among pregnant women in relation to their blood type and to investigate parasitemia severity levels in patients.
The study was conducted in the Kwadon region of Gombe state’s Yamaltu Deba Local Government Area. It is located between latitudes 10°27′ and 10°16’N and longitudes 11°28’E and 11°17’E. The district has a single primary health facility that offers a wide range of services, including antenatal care, malaria diagnosis, and treatment, and functions as a referral health facility for all the nearby communities. Tera, Fulani, Hausa, and Waja are the four main tribes in the region. Kwadon is renowned for its year-round agricultural pursuits.
Ethical approval from Gombe State Ministry of Health was communicated via a letter with the reference number MOH/ADM/621/Vol.1/416. Prior to the research, consent of the Local Government Primary Health Care Department, Yamaltu Deba was sought for using their facility as the recruitment center and its patients as the study subjects for the research. After permission issuing, the importance of the research and the need for active participation by giving a blood sample and other essential information were discussed with each subject. If verbally consented, the subject was included in the study.
This study considers only pregnant women who reported themselves to Kwadon Primary Health Care for antenatal and were voluntarily willing to participate in the study.
The actual sample size was determined (formula 1) [13]
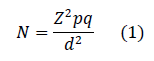
Where:
N: number of subjects to be included
Z: z-score at 95% confidence interval (1.96)
p: prevalence rate 50% (0.5)
q: 1- p
d: error rate (0.05)
This formula is used when the studied community is larger than 10000, and the outcome in the current research was n=384
Blood samples were collected using the venepuncture technique, and safety procedures were adopted. The upper arm was tied with a tourniquet, and the puncture site was sterilized using cotton wool moistened with 70% alcohol. The blood was drawn with a sterile needle attached to a 5ml plastic syringe. 2.0-2.5ml of the venous blood sample was collected from the median cubital vein of each participant, transferred into Ethylene Diamine Tetra Acetic acid (EDTA) containers, and gently mixed with the EDTA.
Staining and examination of slides
Thin and thick films were prepared on oil-free microscopic slides. The thick film was then fixed with methanol and allowed to air-dry. The dried films were stained with 10% Giemsa for 10 minutes before being examined in an oil immersion under 100× objective lens on a microscope
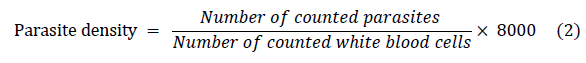
Determination of parasite density
Thin films were used to identify the species and infective stages of the parasites, while thick films were used to compute parasite densities using the WHO technique (formula 2). After 200 microscopic fields were examined, films were deemed negative if no parasites were discovered. A senior biomedical scientist independently cross-examined the slides for the purposes of quality control and assurance, and the results were compared.
ABO/ Rhesus grouping
Commercially available monoclonal anti-A, anti-B, and anti-D (anti-sera + Agappe Diagnostics TD, India) were used for ABO/Rhesus blood grouping. The three plate boxes each contained one drop of each grouping antisera. Each plate box containing the anti-sera received one drop of the test blood sample. Then, the suspension was well mixed by tapping the plate. Samples were kept at room temperature for an hour without disturbing. The plates were then checked for agglutinations.
All data were analyzed using a statistical Package for Social Sciences (SPSS) version 20.0. Chi-square was used to test for associations between the variables, and statistical significance was set at P≤0.05.
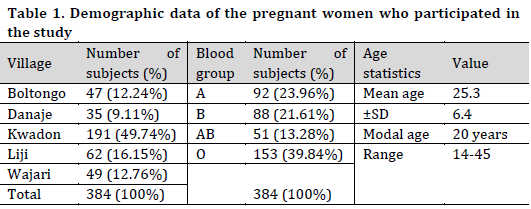
A total of 384 consented pregnant women from five different villages comprises of Kwadon (49.74%), Liji (16.5%), Wajari (12.76%), Boltongo (12.34%), and Danaje (9.11%), all from Yamaltu-Deba Local Government were enrolled in the study (Table 1). The age of the study subjects ranged from 14-45 years, with a mean age of 25.3±6.4. Most subjects (30.5%) were in the age range of 16-20 years, more than half were in their third trimester, and the greater proportion of the participants (39.84%) belonged to blood group O.
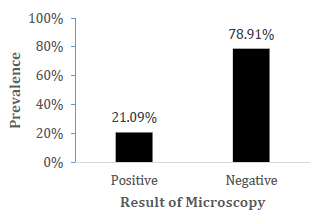
Out of the examined blood samples, an overall prevalence of 81 (21.09%) was recorded (Fig 1).
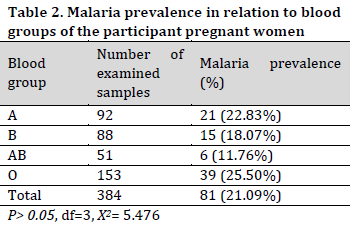
The highest malaria prevalence of (25.5%) was recorded in participants with blood group O, while subjects with blood group A, B and AB recorded a prevalence of 22.83%, 18.07%, and 11.76%, respectively (Table 2). Statistically, there was no significant difference (P>0.05, df=3, X2=5.476) in the level of malaria infection among different blood groups.
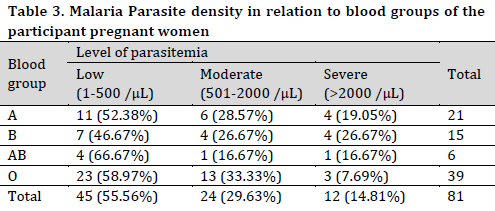
Parasite density results revealed that most cases (55.6%) had a low level of parasitemia and all blood types showed similar prevalences in this level of parasitemia ranging between 46.67% and 58.97% of cases across blood groups. On the other hand, 29.63% and 14.81% of the patients experienced moderate and severe parasitemia, respectively (Table 3). It is worth noting that O blood group showed the least severe infection percentage (7.69%).
Despite the fact that malaria is preventable and can also be controlled [13], especially among pregnant women who usually receive malaria preventives, such as Insecticide-treated bed nets (ITNs) and recommended chemoprophylactic drugs such as antifolate (Sulfadoxine Pyramethamine) for free [14], the disease continues to be prevalent among pregnant women and claim their lives. Out of the 384 participated pregnant women in this study, an overall prevalence of 21.09% was recorded. This result is similar to the findings of [15], who reported an overall prevalence of 21.6% of malaria infection from moderate and high transmission settings in Ethiopia, but slightly lower than 29.5% and far lower than 62.0% malaria prevalence reported by [16] and [17] from Maiduguri and North-Central Nigeria, respectively. Similar outcomes in Gombe and Maiduguri are expected as the two study areas are located in the same region (Northeast) of the country and share a boundary.
For the past four decades, various researchers have shown a solid correlation between blood groups and malaria infection [18]. In this study, the highest malaria prevalence of 25.50% was reported in blood group O. This observation is similar to the findings of [16], who also reported the highest malaria prevalence in O blood type. On the other hand, the current results showed that the least prevalence of severe parasitemia was found in patients of the O blood group (7.69%). This finding is in accordance with the existing knowledge that shows a significantly decreased risk of severe malaria infection in those with O blood type [19], which is partly due to the inability of the parasite (Plasmodium falciparum) to infiltrate this blood type [20]. It is reported that group O patients are less likely to experience a complicated form of falciparum malaria due to a lack of antigens A and B, affecting cytoadherence, rosetting, and sequestration. Therefore, blood group O individuals are less likely to suffer from complicated (severe) falciparum malaria [12]. Nevertheless, decreased susceptibility of blood group O to malaria parasite does not mean complete absence of the parasite in the infected group O erythrocyte but only hinders the manifestation of the severe form of the disease [21]. In other words, blood group O does not preclude individuals from getting infected with the parasite but rather protects them from having a severe form of the disease due to reduced rosette formation while other blood groups cannot [22]. Therefore, differences in the antigens found in the infected erythrocyte play no significant role in non-complicated cases of malaria since different blood groups can equally be infected. However, the difference could be attributed to the prevailing predisposing factors of the diseases, not the blood group or antigens on the infected erythrocyte. Nevertheless, reporting the highest malaria prevalence from subjects having blood group O in the presence study might be attributed to the fact that most of the subjects belong to that blood group. For instance, [23] reported the highest malaria prevalence among subjects with blood group A from Jos Plateau state, Nigeria.
More than 85% of the study subjects, irrespective of their blood group, had either low (55.56%) or moderate (29.63%) parasitemia. This observation was expected since the study area is among the areas where the disease is endemic. Furthermore, most malaria control programs are still not adequately designed to target and reach the expected target and vulnerable groups in rural communities either due to a lack of adequate resources or political will to address the menace.
Malaria infection is prevalent in the study area, though with low prevalence. The highest malaria prevalence was reported from subjects with blood group O, and less than 15% of the total cases had severe parasitemia.
Massive awareness campaigns on malaria preventive measures among the pregnant women in the study area should be conducted to target zero prevalence. In addition, further research should be conducted to determine the impact of the disease among the subjects concerning other genetic variables and biological factors.
Conflict of interest statement
The authors declared no conflict of interest.
Funding statement
The authors declared that no funding was received in relation to this manuscript.
Data availability statement
The authors declared that all related data are included in the article.